Premarin dosages: 0.625 mg
Premarin packs: 14 pills, 28 pills, 56 pills, 84 pills, 112 pills
Premarin 0.625 mg buy with amex
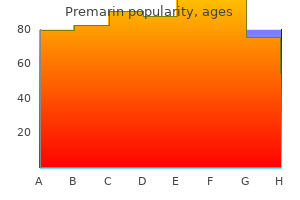
Hebert 1107 Hemangiomas are a neoplastic proliferation of endothelial cells which may be usually benign but have been related to native tissue damage menopause gas bloating buy discount premarin 0.625 mg online, useful impression womens health specialist yuma az order premarin 0.625 mg online, and ulceration. The true incidence of the illness is unknown but is reported as 5% in Caucasian infants. Hemangiomas happen more regularly in Caucasian feminine infants with a predilection for premature infants, especially of low start 1108 weight or a quantity of gestations. Most hemangiomas come up spontaneously during infancy, however an autosomal-dominant pattern of inheritance has rarely been reported as nicely. Management Strategy Cutaneous hemangiomas seem within the first few weeks of life and attain 80% of size by three months, with spontaneous involution typically by age 10. About half of the youngsters with hemangiomas may have normal skin after involution, however the remaining may have residual adjustments, together with telangiectasias, atrophy, fibrofatty residuum, and scarring. Differentiating benign widespread hemangiomas from other vascular anomalies is crucial, because the pathophysiology, therapy modalities, and prognoses are considerably totally different. Although the pure course of hemangiomas is self-limited and is commonly treated with active nonintervention, pharmaceutical intervention is indicated for hemangiomas that ulcerate, grow rapidly, compress, obstruct, or distort important constructions, such as the larynx, eyes, ears, and nose. In addition, hemangiomas associated with systemic involvement and large disfiguring facial hemangiomas must be treated. Medical administration is generally centered on the administration of topical and systemic beta-blockers or corticosteroids. The first case report of a hemangioma being efficiently treated with propranolol was revealed in 2008. Adverse occasions embrace the masking of hypoglycemia, hypotension, and bradycardia, which can be minimized by administering the treatment after feeding and monitoring the center rate and blood pressure after dose will increase. Timolol, available as an answer or a gel, has been shown in small randomized medical trials to be protected and effective for superficial childish hemangiomas with twice-daily topical utility. Prednisone or prednisolone can be given at doses from 2 to 4 mg/kg day by day for 2 to 6 months and then progressively tapered over a number of months. Stopping treatment before sufficient therapeutic response may lead to rebound growth. Reported risks include hypothalamopituitary�adrenal axis suppression, development delays, pseudotumor cerebri, infections, and avascular bone necrosis. Surgical excision, either alone or in combination with corticosteroids, may be employed in certain circumstances. For the exceptional recalcitrant hemangioma, different remedies embrace cyclophosphamide, vincristine, bleomycin, and embolization. Doppler ultrasonography is a low-cost, noninvasive methodology to verify the prognosis of a vascular anomaly, monitor therapeutic response, or preclude the involvement of visceral organs. Hemangiomas may be differentiated from vascular malformations on ultrasonography by distinguishing options such as the presence of a solid tissue mass. On T2weighted images, hemangiomas have the characteristic look of multiple lobules, similar to a bunch of grapes. Immunohistochemical staining can function a useful adjunct to distinguish between infantile hemangiomas and different widespread vascular malformations or vascular neoplasms that present throughout infancy. First-Line Therapies Oral propranolol is the mainstay of remedy for life-threatening or endangering hemangiomas with active nonintervention or topical timolol reserved for relatively uncomplicated cases. A randomized, managed trial of oral propranolol in infantile hemangioma Leaute-Labreze C, Hoeger P, Mazereeuw-Hautier J, Guibaud L, Baselga E, Posiunas G, et al. A randomized, double-blind, multicenter, two-stage adaptive trial of 460 infants to assess the efficacy of oral propranolol in treating infantile hemangiomas. In the first stage, the infants had been randomized to obtain both a placebo or considered one of 4 propranolol regimens of both 1 mg/kg/day or three mg/kg/day of propranolol for a duration of three or 6 months. After an interim analysis, new infants had been treated with both a placebo or 3 mg/kg/day of propranolol for six months. Sixty % of all infants receiving this regimen had complete or nearly full decision of the goal hemangioma. A multidisciplinary consensus conference reviewed the present analysis on the utilization of oral propranolol for the treatment of childish hemangiomas, with a primary goal of formulating a standardized set of tips that dermatologists could observe. Based on the evidence, a beginning dose of 1 mg/kg/day divided three times day by day with a titration to a target dose of 2 mg/kg/day was recommended. A whole of 103 sufferers previously started on oral propranolol between September 2008 and May 2013 had been retrospectively assessed for attainable psychomotor developmental delay attributable to the medication. Data had been collected from the Dutch Well Child Preventive Health Care Clinics and interpreted using the Van Wiechen scheme. Overall examine results detected no evidence of psychomotor developmental delay in infants handled with propranolol for infantile hemangiomas. Topical timolol maleate therapy of childish hemangiomas Puttgen K, Lucky A, Adams D, Pope E, McCuaig C, Powell J, et al. This multicenter retrospective cohort examine of 731 patients evaluated the efficacy of topical timolol by scoring digital pictures of the childish hemangioma utilizing a visible analog scale for colour, dimension, extent, and quantity. The mean age at initiation of remedy was eight months, with 85% of sufferers dosed at 0. A retrospective review of 34 patients with hemangiomas handled with class I topical steroids showed good response in 35%, partial response in 38%, and no response in 27%. In this retrospective examine, 155 hemangiomas of the head and neck area treated with intralesional corticosteroid injections (three to six injections of triamcinolone acetonide 10 mg/mL at month-to-month intervals, with an average of 4 injections per lesion) have been analyzed. At the 1month go to, 85% of hemangiomas showed higher than 50% discount, with superficial hemangiomas exhibiting probably the most enchancment. Perioral hemangiomas appeared essentially the most recalcitrant to intralesional corticosteroid treatment. This meta-analysis of 10 case series with 184 patients analyzed the efficacy of systemic corticosteroids in the remedy of cutaneous 1114 hemangiomas. The imply response rate was 84%, and the imply rate of rebound growth after therapy cessation was 36%. Treatment with larger doses of corticosteroids resulted in a better response rate but greater adverse events. The average incidence of unwanted effects was 35% (behavior modifications, irritability, cushingoid look, and transient development delay). A retrospective case evaluation of 74 sufferers handled surgically was analyzed to evaluate outcomes based on tumor-related scientific options. The finest candidates for emergency surgical procedure had been nonresponders to pharmacologic therapy with segmental periorbital hemangiomas, whereas these undergoing elective surgery have been patients with localized lip, nasal, or eyelid hemangiomas in the proliferative phase. Although most patients with infantile hemangiomas must be managed with pharmacotherapy, surgery remains an essential option. A 21-month-old toddler with a large, deep hemangioma within the beard distribution, necessitating a quantity of hospital admissions for respiratory and feeding difficulties, was treated with vincristine after failing to reply to systemic corticosteroid therapy. Although there are literature reviews of success achieved with vincristine, the information are anecdotal at finest. Eighteen youngsters (median age of 18 weeks) treated with imiquimod 5% cream three or five times weekly for a mean of 17 weeks confirmed improvement in superficial hemangiomas and accelerated ulcer therapeutic; no change was seen in deep hemangiomas. Unfortunately, this examine lacked a control arm, and the results may represent the natural course of untreated infantile hemangiomas. Role of intralesional bleomycin in the therapy of sophisticated hemangiomas: prospective clinical research Omidvari S, Nezakatgoo N, Ahmadloo N, Mohammadianpanah M, Mosalaei A.
Purchase 0.625 mg premarin otc
Nasal swabs from the patient and immediate family members must be performed to determine asymptomatic nasal carriers of Staphylococcus aureus pregnancy jaw pain order 0.625 mg premarin visa. In the case of outbreaks on wards and in nurseries womens health evanston 0.625 mg premarin purchase mastercard, well being care professionals must also be swabbed. Failure of first-line remedy suggests the presence of bacterial resistance or poor affected person compliance. The alternative of antibiotic ought to be primarily based on the sensitivities of organisms cultured from the pretreatment swab. In recurrent circumstances, think about the potential for nasal or pharyngeal colonization with pathogenic S. This may require eradication by the use of a systemic antibiotic in conjunction with the nasal software of a topical antibiotic and an antiseptic pores and skin cleanser. Personal clothing and underwear, towels, washcloths, and mattress linens are washed daily for five days. Grattan, and Frances Lawlor Inducible urticarias 1266 About 25% of patients with continual urticaria have a definable and reproducible inducing trigger that distinguishes them from these with spontaneous urticaria and urticarial vasculitis. More than one inducing stimulus elicits urticaria in some patients, and inducible urticarias can overlap with spontaneous urticaria. Physical urticarias caused by a physical stimulus (symptomatic dermographism, delayed strain, warmth and chilly contact and solar urticarias, and vibratory angioedema) at the second are included inside the inducible urticarias. Management Strategy Pharmacologic the presentation of inducible urticarias may range in morphology and severity. Milder forms might require little more than avoidance of triggers and a preemptive dose of H1 antihistamine earlier than anticipated exposure, whereas a really severe assault involving anaphylaxis could doubtlessly require emergency remedy with intramuscular epinephrine (adrenaline). Acute displays of extreme inducible urticaria could require short courses of oral corticosteroids. Drug management should be guided by the diploma of incapacity or impairment in high quality of life. Cold tolerance induction in cold urticaria and exercise tolerance induction in cholinergic urticaria has been described but is tough to obtain and sustain. Anaphylaxis may hardly ever outcome from train after a heavy food load or consuming sure foods. Up-dosing of second-generation H1 antihistamines is now extensively practiced, although sedation at higher-than-licensed doses is a potential danger. Therapeutic effects of cetirizine in delayed pressure urticaria: clinicopathological findings Kontou-Fili K, Maniatakou G, Demaka P, Gonianakis M, Palaiologos G, Aroni K. A double-blind, placebo-controlled study in eleven sufferers, exhibiting a discount in weight-induced wheal space and lesional eosinophil numbers on cetirizine 10 mg three times every day. High-dose desloratadine decreases wheal quantity and improves chilly provocation thresholds in contrast with standard-dose remedy in patients with acquired cold urticaria: a randomized, placebo-controlled, cross-over examine Siebenhaar F, Degener F, Zuberbier T, Martus P, Maurer M. Fourfold up-dosing a second-generation antihistamine has extra inhibitory results on wheal formation in cold urticaria. Rupatadine and its effects on symptom control, stimulation time, and temperature thresholds in sufferers with acquired cold urticaria 1269 Metz M, Scholz E, Ferr�n M, Izquierdo I, Gim�nez-Arnau A, Maurer M. A crossover, randomized, double-blind, placebo-controlled examine of double-dose rupatadine, a second-generation H1 antihistamine. There was also a big enchancment in critical cold stimulation time and critical temperature threshold. Anti-immunoglobulin E remedy of sufferers with recalcitrant bodily urticaria Metz M, Altricher S, Ardelean E, Kessler B, Krause K, Magerl M, et al. In this double-blind, crossover research, 19 patients had been randomized to remedy with cetirizine 10 mg at night plus either ranitidine one hundred fifty mg twice day by day or placebo. There was an increase in whealing threshold with additional H2 blockade, but no subjective profit on itch. Addition of an H2 to an H1 antihistamine may present higher management of some inducible urticarias despite the shortage of trial proof. Seventeen male sufferers handled with danazol 200 mg thrice every day in a double-blind crossover examine had sustained improvement in the variety of exercise-induced wheals over 12 weeks. Anabolic steroids ought to only be thought-about for severe cholinergic urticaria not responding adequately to up-dosed H1 antihistamines, due to their potential for virilization and hepatotoxicity. Successful remedy of cholinergic urticaria with antiimmunoglobulin E remedy Metz M, Bergmann P, Zuberbier T, Maurer M. One affected person with highly symptomatic cholinergic urticaria who had not responded to a quantity of antihistamines, montelukast, and propranolol made an entire and sustained response to omalizumab 300 mg each 2 weeks. A patient with disabling cholinergic urticaria was fully unresponsive to omalizumab subcutaneously at 300 mg every 2 1273 weeks for four months. Clinical expertise with omalizumab for cholinergic urticaria signifies that it can be extremely effective however not each patient will respond. Severe cholinergic urticaria efficiently handled with scopolamine butylbromide along with antihistamines Ujiie H, Shimizu T, Natsuga K, Arita K, Tomizawa K, Shimizu H. Although this case report means that anticholinergics could also be profitable for cholinergic urticaria, the overall experience with this class of drugs is disappointing, and unwanted effects often outweigh any advantages. A trial of omalizumab in a 12-year-old atopic lady with more and more severe cold-contact urticaria led to full resolution of her signs over 5 months, however her signs recurred when she missed two doses of omalizumab. An rising variety of reviews illustrate the nice response that some patients with chilly urticaria have with omalizumab given off-license. A case report of a affected person with acquired cold-contact urticaria responding subjectively and objectively to montelukast 10 mg daily after only four days. Two sufferers with severe cold-contact urticaria improved subjectively and objectively on a combination of cetirizine 10 mg once 1274 day by day and zafirlukast 20 mg twice daily. Further research are required to clarify what place (if any) leukotriene receptor antagonists have in the administration of antihistamine-unresponsive chilly urticaria. Acquired chilly urticaria: medical picture and update on diagnosis and therapy Siebenhaar F, Weller K, Mlynek A, Magerl M, Altrichter S, Vieira Dos Santos R, et al. The authors declare that occasional patients reply to high-dose antibiotics even if no underlying infection could be detected, but personal expertise suggests little or no profit. Cold desensitization in four sufferers with severely disabling cold urticaria resulted in symptom-free follow-up starting from 4 to 14 years. Nine of 23 patients desensitized with cold water immersions 15 years earlier responded to a questionnaire survey. Only considered one of them was capable of continue the cold baths for 6 months, two for 3 months, and the others stopped almost instantly. This report introduces a little realism concerning the probability of cold desensitization being an efficient and well-tolerated long-term therapy for cold-contact urticaria. Heat urticaria: a revision of printed instances with an replace on 1275 classification and management Pezzolo E, Peroni A, Gisondi P, Girolomoni G. Effective remedy of various phenotypes of chronic urticaria with omalizumab: case stories and review of literature Kasperska-Zajac A, Jarzb J, erdziska A, Bk K, Grzanka A. Omalizumab is more and more being reported as a successful therapy of delayed stress urticaria. It can be effective for patients with continual spontaneous urticaria and delayed pressure urticaria.
Premarin 0.625 mg discount on line
Treatment of linear IgA bullous dermatosis of childhood with flucloxacillin Alajlan A menstrual twice in one month premarin 0.625 mg purchase with mastercard, Al-Khawajah M menstrual 6 months purchase premarin 0.625 mg on line, Al-Sheikh O, Al-Saif F, Al-Rasheed S, AlHoqail I, et al. Antibiotics have been used largely in childhood disease and are an affordable option because of their low toxicity. Successful remedy of linear IgA illness with salazosulphapyridine and intravenous immunoglobulins Goebeler M, Seitz C, Rose C, Sitaru C, Jeschke R, Marx A, et al. A newborn with skin involvement had life-threatening respiratory compromise from illness affecting the larynx, subglottis, trachea, and esophagus. An 8-year-old boy demonstrated a dramatic response with thalidomide with whole clearance in 1 month, and whereas on therapy he was disease free for 1 year. The authors postulate that thalidomide works by inhibition of interleukin-12, which is a potent proinflammatory cytokine. Linear IgA illness: successful software of immunoadsorption and evaluation of the literature Kasperkiewicz M, Meier M, Zillikens D, Schmidt E. Immunoadsorption has been beforehand efficiently utilized in severe and/or in any other case treatment-resistant IgG-mediated immunobullous problems. It usually presents as a sclerotic region, often surrounding venous ulcers, above the medial malleolus on the lower leg. Often, clinicians mistake the acute type for cellulitis, phlebitis, erythema nodosum, inflammatory morphea, or panniculitis. The persistent variant, which is strongly associated with venous insufficiency, is densely indurated and fewer painful than the acute kind. Management Strategy the current therapy of choice is the mix of stanozolol and compression therapy. Stanozolol is contraindicated in sufferers with uncontrolled hypertension and heart failure. Of note, although stanozolol is not commercially available in the United States, danazol has been used in its place. However, stanozolol is still out there in Europe, and its purchase is unregulated online. Pentoxifylline is another that stimulates fibrinolysis but could trigger gastrointestinal upset. Other remedies, such as antibiotics, antiinflammatory agents, antimetabolites, and long-term cimetidine, have additionally been proposed. Intralesional triamcinolone, platelet-rich plasma, and topical capsaicin may be helpful. In the subcutis, there was lobular and septal panniculitis with eosinophils, fibrin thrombi, and purpura. Most cases present pseudoxanthoma elasticum�like elastic fiber calcification throughout the septae. Results of duplex scanning of 205 decrease extremities with varices: 106 not previously operated and ninety nine previously operated for varicose veins Egeblad K, Baekgaard N. Excision of lipodermatosclerotic tissue: an efficient remedy for non-healing venous ulcer Ahnlide I, Bjellerup M, Akesson H. In seven cases, laser Doppler scanning confirmed a rise in blood move in lipodermatosclerotic pores and skin, which decreased after surgical removing of the affected area. The authors counsel open-toe and below-the-knee graded stockings, with 30- to 40-mm Hg strain. Patients taking stanozolol ought to be rigorously monitored for excessive fluid retention, hirsutism, acne, liver operate, and plasma fibrinogen concentration. Stanozolol is contraindicated in patients with uncontrolled hypertension or congestive heart failure. In an open trial of 17 sufferers, stanozolol 2 mg twice day by day, without compression, decreased pain and dermal thickness. Surgical correction of superficial venous reflux (saphenous vein ablation) with compression lowered ulcer recurrence at four years in contrast with remedy with compression alone. Pentoxifylline is a dimethylxanthine by-product that increases purple blood cell flexibility, alters fibroblast physiology, and stimulates fibrinolysis. The dose of 400 mg three times every day may be increased to 800 mg three times day by day if no enchancment happens. Excision of lipodermatosclerotic tissue: an efficient treatment for nonhealing venous ulcer Ahnlide I, Bjellerup M, Akesson H. Surgical elimination of ulcer and lipodermatosclerosis followed by 1542 split-skin grafting (shave therapy) yields good long-term results in "non-healing" venous leg ulcers Schmeller W, Gaber Y. A retrospective chart review of 28 patients confirmed enchancment in ache, erythema, edema, and induration after one to three intralesional injections of 5 to 10 mg/mL triamcinolone. Lipodermatosclerosis: enchancment famous with hydroxychloroquine and pentoxifylline Choonhakarn C, Chaowattanapanit S. A retrospective chart evaluate of 32 patients showed improvement in ache, erythema, edema, and induration after therapy with hydroxychloroquine (maximum <6. An acute case of lipodermatosclerosis efficiently handled with danazol Hammerman S, Mamakos L, Falanga V. Danazol is an anabolic androgen, with fibrinolytic exercise similar to stanozolol. Lipodermatosclerosis: profitable treatment with danazol Hafner C, Wimmershoff M, Lanthaler M, Vogt T. Treatment of lipodermatosclerosis with oxandrolone in a affected person with stanozolol-induced hepatotoxicity Segal S, Cooper J, Bolognia J. Oxandrolone is another anabolic androgen just like stanozolol with recognized fibrinolytic exercise however with a decrease incidence of hepatotoxicity. Oxandrolone 10 mg twice daily lowered ache and induration of the legs with 3 months of remedy. In this prospective research, sclerotherapy with 1% to 3% polidocanol foam with compression is superior to compression alone for venous ulcer therapeutic. Hypodermatitis sclerodermiformis and strange acid-fast bacteria Cantwell A, Kelso D, Rowe L. There is little proof to support the usage of antibiotics, 1544 antiinflammatory agents, or antimetabolites. Refractory lipodermatosclerosis handled with intralesional platelet-rich plasma Jeong K, Shin M, Kim N. Topical capsaicin for the treatment of acute lipodermatosclerosis and lobular panniculitis Yosipovitch G, Mengesha Y, Facliaru D, David M. The unaffected normal-colored islands of pores and skin are the areas where blood provide is sufficient; in the 1547 community areas the supply is inadequate. This commonly occurs on the legs, arms, and trunk, but can be diffuse, and is extra pronounced after exposure to chilly. No specific remedy is required for this condition besides avoidance of chilly exposure, protection from chilly publicity with heat clothing, and rewarming the affected space. Cutis marmorata telangiectatica congenita is uncommon and presents at delivery or quickly after delivery.
Premarin 0.625 mg buy discount online
Direct confrontation ought to be averted menstrual molimina premarin 0.625 mg purchase mastercard, if attainable pregnant safe 0.625 mg premarin, and instead, a supportive setting and a stable physician�patient therapeutic alliance ought to be fostered, often initially through quick (so as not to "burn out" the dermatologist) however frequent (so as to satisfy the patient) workplace visits. Once the affected person establishes trust within the physician by means of a stable relationship, the physician could assist the patient acknowledge the psychosocial impression of the disorder and advocate session with a psychiatrist or psychotherapy. However, this approach should be tried only if the clinician feels that the therapeutic rapport is robust sufficient to obtain chance of success somewhat than being misinterpreted negatively and defensively by the affected person. Most sufferers with dermatitis artefacta will have a continual waxing and waning course of illness. Regular visits, whether or not or not lesions are current, will assist the affected person feel cared for and diminish the need for self-mutilation as a call for help. This handbook is an up-to-date evaluation of the diagnosis and therapy of dermatitis artefacta. This article describes widespread dermatologic presentations of psychopathology, together with dermatitis artefacta. Dermatitis artefacta in pediatric sufferers: expertise at the National Institute of Pediatrics Saez-de-Ocariz M, Orozco-Covarrubias L, Mora-Maga�a I, DuranMcKinster C, Tamayo-Sanchez L, Gutierrez-Castrellon P, et al. It is considered rare in kids; 12 of the 29 patients reported had an associated continual illness, and 7 exhibited mild mental retardation. The medical and histopathologic options, diagnostic aids, approach to therapy, and prognosis for dermatitis artefacta are discussed in this case report. A retrospective analysis of fifty seven sufferers with dermatitis artefacta seen in a dermatology division Nielsen K, Jeppesen M, Simmelsgaard L, Rasmussen M, ThestrupPedersen K. This retrospective analysis of fifty seven sufferers reported the next findings: when self-infliction was advised as the potential cause of illness to sufferers (n = 30), just one affected person agreed to see a psychiatrist, and two thirds denied self-infliction or discontinued treatment. The three most typical lesion types were skin ulcers (72%), excoriations (46%), and erythema (30%). Of the 57 patients, 61% have been handled with anxiolytic or antidepressant drugs. In 32 patients, occlusive dressings were administered, and the lesions showed improvement besides in two cases. Palliative dermatologic measures similar to occlusive bandages, ointments, or placebo medication, as well as hospitalization that features bathing and massaging by nurses, can have a therapeutic impression on the psychiatric downside by symbolizing the medical attention and care the affected person with dermatitis artefacta is craving. This article briefly evaluations therapy for dermatitis artefacta, including the usage of aripiprazole. Second-Line Therapy Treatment of self-mutilation with olanzapine Garnis-Jones S, Collins S, Rosenthal D. Three patients had been efficiently treated with low-dose olanzapine when multiple other therapies (including antidepressants and other antipsychotics) failed. More than 85% of patients have an associated celiac illness that spans the spectrum of intestinal histologic severity. The pores and skin disease also presents with a spectrum of severity, ranging from minimal pruritic papules on the elbows and knees to extreme, intensely pruritic vesicular lesions over multiple extensor surfaces. Histologically, vesicle formation on the dermal-epidermal junction and infiltration of dermal papillary tips with neutrophils happens in two thirds of the instances, but different cases could present solely nonspecific inflammatory findings. Direct immunofluorescence exhibits granular or fibrillar IgA localized within the dermal papillary ideas or along the basement membrane of perilesional skin. Elevated ranges of IgA antibodies to tissue transglutaminase are characteristic of celiac illness, correlate with the degree of intestinal inflammation, and reduce with gluten restriction. If medical remedy with dapsone or sulfapyridine is chosen, the cutaneous lesions may be nicely controlled. Occasionally, some patients (10%�20%) will enjoy a spontaneous remission with out medicine or dietary restriction. Initial treatment with dapsone 25 mg daily will enhance pruritus within 24 to forty eight hours and the papulovesicular lesions within 1 week in adults. Maintenance remedy is then adjusted on a weekly foundation to preserve adequate suppression of symptoms. Despite enough dapsone dosages, outbreaks of facial and scalp lesions are widespread. The advantages of gluten restriction include a discount of dapsone dosage and its attendant problems, improvement of gastrointestinal symptoms (which range from cramping pain to overt diarrhea), and a therapy aimed at the cause somewhat than the signs of the illness. Recently gluten-free foods have turn into extra out there, and affected person help teams supply in depth info. Sulfapyridine is began at 500 mg three times a day and is normally increased to a maximum maintenance dose of 1. Dapsone may produce a drug hypersensitivity syndrome with liver toxicity in the first three to 12 weeks. Hepatocellular toxicity can also occur in a doserelated fashion, especially with doses higher than 2 mg/kg. There are three main hematologic toxicities of dapsone: hemolysis, methoglobinemia, and agranulocytosis. Methoglobinemia is usually mild and never problematic unless the affected person has underlying cardiopulmonary problems. Virtually all patients have at least some extent of hemolysis, and a fall of the hemoglobin of 1 to three g/dL is to be expected. A compensatory reticulocytosis occurs and may be monitored with a reticulocyte depend. Hemolysis could additionally be extreme in sufferers with glucose-6-phosphate dehydrogenase deficiency. Glucose-6-phosphate dehydrogenase ranges must be evaluated in blacks and people of Southern Mediterranean origin before the initiation of therapy to keep away from potentially catastrophic hemolytic anemia. Complete blood count and liver function tests ought to be checked each 2 to 3 weeks for the primary three months after which every three to 6 months thereafter. A long-term gluten-free diet instead treatment in severe forms of dermatitis herpetiformis Nino M, Ciacci C, Delfino M. A complete of 89% of patients on diet and dapsone had remission of skin illness (70% of severe patients), and 11% had been improved. Sulfasalazine, which is extra readily available, is metabolized to 5-amino-salicylic acid and sulfapyridine. Patients have been reported to respond to sulfasalazine, 2 to four g/day administered twice day by day. It involves the ingestion of amino acid and carbohydrate alone and is commercially available as Vivonex. It produces rapid healing of the gut and reduction of cutaneous signs but was designed for tube feeding and is considered unpalatable by many. The authors recommend that colchicine may be used when dapsone or sulfapyridine is contraindicated. It is related to a excessive threat 694 for native recurrence and widespread subclinical extension. It happens most frequently in adults aged 20 to 50 years; pediatric and infantile cases, particularly when congenital, are rare.
Diseases
- Carpotarsal osteochondromatosis
- Distal myopathy
- Neurocysticercosis
- Calvarial hyperostosis
- Rhabdomyosarcoma, alveolar
- Exercise induced anaphylaxis
- Cystic hygroma
- Laryngeal carcinoma
- Pitt Rogers Danks syndrome
- Syndactyly Cenani Lenz type
Buy 0.625 mg premarin amex
Successful therapy of pityriasis rubra pilaris with oral vitamin A in oil (Chocola A) for an 18-month-old baby Kan Y pregnancy night sickness buy discount premarin 0.625 mg on line, Sumikawa Y women's health clinic waco tx 0.625 mg premarin purchase with visa, Yamashita T. Skin lesions resolved after 2 months on that dose, but recurred 2 weeks after the vitamin A was discontinued. Management Strategy There are few therapeutic trials for this situation, and case sequence are only small. Topical corticosteroids are solely reported as efficient anecdotally in textbooks somewhat than in research. The response appears to be unpredictable, however, and the total dose required is extremely variable. Antibiotics appear to be more useful in youngsters, sometimes utilized in combination remedy. For severe or refractory circumstances methotrexate, photochemotherapy, and etanercept have all been described as efficient in small numbers of patients. Specific Investigation � Consider skin biopsy Although a pores and skin biopsy is usually unnecessary in clinically obvious cases, it may be useful before commencing systemic remedy with more potential opposed effects. These reviews are likely to come from endemic areas, and so investigation for a triggering infection is unnecessary in cases with out proof of specific an infection. Five of the latter had subsidence of skin lesions after pyrimethamine and sulfapyrimidine therapy. First-Line Therapies Comparative studies of remedies for pityriasis lichenoides Gritiyarangsan P, Pruenglampoo S, Ruangratanarote P. The first group of 8 were given topical corticosteroid, and half had a partial or complete response. The second group have been also given oral tetracycline, and the bulk had a partial response. Is narrowband ultraviolet B monotherapy efficient within the therapy of pityriasis lichenoides The authors state that the distinction in response is insignificant and that each options are acceptable. Second-Line Therapy 2117 Pityriasis lichenoides: the variations between kids and adults Wahie S, Hiscutt E, Natarajan S, Taylor A. In this retrospective examine only two of eight kids cleared with erythromycin, whereas three out of 4 adults cleared without relapse. The median age of onset was 60 months and median period was 20 months (range 3�132 months). Childhood pityriasis lichenoides and oral erythromycin Hapa A, Ersoy-Evans S, Karaduman A. Pityriasis lichenoides chronica induced by infliximab, with response to methotrexate L�pez-Ferrer A, Puig L, Moreno G, Camps-Fresneda A, Palou J, Alomar A. Adalimumab-induced pityriasis lichenoides chronica that responded well to methotrexate in a patient with psoriasis 2119 Mart�nez-Peinado C, Gal�n-Guti�rrez M, Ruiz-Villaverde R, Solorzano-Mariscal R. Photochemotherapy for pityriasis lichenoides: three circumstances Panse I, Bourrat E, Rybojad M, Morel P. She was commenced on etanercept with marked improvement in pruritus and irritation after 2 months and no new lesions after 4 months when therapy was stopped. Conflictingly, there are reviews of etanercept, infliximab, and adalimumab inflicting pityriasis lichenoides. The name refers to the morphology, not the length of the situation, 2123 because a significant proportion of cases regress, with or with out remedy, only to recur. Patients should be warned that relapse is frequent and that recurrent courses of remedy may be required. Management Strategy There are only a handful of managed trials for this situation, and enormous collection are rare. Although a "wait and see" strategy is justifiable in infants, youngsters must be given a 6-week course of high-dose erythromycin. Topical corticosteroids are solely reported anecdotally in textbooks rather than in research. In more extensive or symptomatic disease low-dose methotrexate is useful, and systemic corticosteroids or ciclosporin have additionally been used. In Mucha�Habermann illness, given its severe nature, mixture therapy is usually prescribed. Specific Investigation � Consider skin biopsy A diagnostic pores and skin biopsy is unnecessary in clinically apparent cases but could also be useful to exclude lymphomatoid papulosis or before commencing aggressive systemic therapy. Classically a lichenoid infiltrate is seen within the superficial dermis with parakeratosis in the stratum corneum and keratinocyte necrosis in the epidermis. There 2124 could additionally be pink cell extravasation, together with trapped pink cells in the epidermis, and a lymphocytic infiltration around the dermal vascular plexus and the dermoepidermal junction. Is varicella-zoster virus concerned within the etiopathogeny of pityriasis lichenoides This study advised that pityriasis lichenoides is mediated by a cytotoxic T-cell effector inhabitants. Febrile ulceronecrotic Mucha-Habermann illness: proposed diagnostic criteria and therapeutic analysis 2125 Nofal A, Assaf M, Alakad R, Amer H, Nofal E, Yosef A. Nine improved inside a month, and 2 to 6 months after stopping the drug there was only one recurrence. The remaining 12 sufferers got oral erythromycin 20 to forty mg/kg every day for 1 to 2 weeks, and the response was described as "moderately effective. The first group of eight patients were given topical corticosteroid, and half had a partial or complete response. The second group got corticosteroid plus oral tetracycline, and the majority had a partial response. The third group of eight patients with chronic refractory pityriasis lichenoides got oral methoxsalen 0. Photochemotherapy for pityriasis lichenoides Panse I, Bourrat E, Rybojad M, Morel P. Methotrexate treatment in kids with febrile ulceronecrotic Mucha-Habermann disease: case report and literature evaluation Bulur I, Kaya Erdoan H, Nurhan Saracoglu Z, Arik D. Eleven-year-old male with biopsy-proven Mucha�Habermann disease handled unsuccessfully with 10 days of 32 mg/day methylprednisolone. He was then commenced on methotrexate 15 mg/week with illness resolution at 6 weeks. Resistant pityriasis lichenoides et varioliformis acuta in a 3-yearold boy: successful remedy with methotrexate Lazaridou E, Fotiadou C, Tsorova C, Trachana M, Trigoni A, Patsatsi A, et al. The solely therapeutic strategy that eventually managed to stop the disease evolution was the combination of prednisolone (1 mg/kg for 8 weeks) and methotrexate (5 mg/week for 8 weeks). Successful remedy of cyclosporin A in pityriasis lichenoides et varioliformis acuta preceded by hand, foot and mouth disease Lis-wity A, Michalska-Bakowska A, Zielonka-Kucharzewska A, Pyplacz-Gumprecht A. Treatment with three mg/kg/day cyclosporin A resulted in rapid scientific enchancment and discontinuation after 4 weeks. Treatment with ciclosporin 200 mg day by day produced a rapid response, though prolonged upkeep treatment was required. Pityriasis lichenoides et varioliformis acuta: case report and evaluate of the literature Pereira N, Brinca A, Manuel Brites M, Jos� Juli�o M, Tellechea O, Gon�alo M.
Premarin 0.625 mg purchase without a prescription
Leishmaniasis is a flagellate protozoan disease brought on by many species of the genus Leishmania womens health 21 day bikini body premarin 0.625 mg generic on-line. It may be classified into three medical varieties: visceral (kala azar) womens health 99 weight loss tips premarin 0.625 mg cheap on line, which is probably the most severe kind; mucocutaneous, which may lead to intensive destruction of the 1415 mucous membranes; and cutaneous (Old and New World), which impacts primarily exposed elements of the body, causing ulcers and finally scarring. Leishmaniasis is transmitted primarily by the bite of the contaminated feminine phlebotomine sandfly. However, different possible routes of transmission exist, together with transfusion, needle sharing, congenital, sexual, and person-to-person contact. Cutaneous leishmaniasis mimicking inflammatory and neoplastic processes: a scientific, histopathological and molecular examine of 57 cases Saab J, Fedda F, Khattab R, Yahya L, Loya A, Satti M, et al. Eighteen circumstances presented with a prebiopsy medical analysis that ranged from dermatitis to neoplasm. It has the advantages of being inexpensive and administered by a noninvasive nasal route. It could be given intralesionally with local anesthetic (particularly in youngsters, because of pain) or systemically 10 mg/kg day by day for two weeks. In widespread severe cases it can be given intramuscularly or intravenously in a dose of 10 mg/kg/day for 2 weeks. Side effects appear to be dose related and are extra widespread in sufferers with renal and liver impairment and people with cardiac arrhythmias. Allopurinol has antileishmanial activity, and other oral medicine such as miltefosine, zinc sulfate, rifampin, doxycycline, and azoles are additionally helpful. Topical preparations corresponding to paromomycin ointment and 5% imiquimod show appreciable therapeutic potential. The aspirate can then be despatched for culture or histology, which exhibits Leishman�Donovan bodies inside macrophages using Giemsa stain. The gold- normal medium for tradition is Novy�MacNeal�Nicolle, with positive results in 1 to three weeks, or Schneider Drosophila medium, which supplies positive results in 1 week. Microculture is a model new tradition medium that has higher carbon dioxide concentrations and decrease oxygen and pH, which inspires extra speedy amastigote to promastigote differentiation. A mixture of intramuscular meglumine antimoniate 20 mg/kg/day plus intralesional meglumine antimoniate zero. Intralesional antimony for single lesions of Bolivian cutaneous leishmaniasis Soto J, Rojas E, Guzman M, Verduguez A, Nena W, Maldonado M, et al. A randomized, open-label trial of eighty sufferers in Bolivia divided sufferers into three groups, one receiving both intralesional antimony, cryotherapy, or placebo. At 6 months the treatment rate was 70% 1420 for the antimony, 20% for cryotherapy group, and 17% for placebo. Intravenous or intramuscular pentamidine isethionate (4 mg/kg) on alternate days cured the lesions within 1 to 3 months. Sixty-four sufferers were enrolled: 32 acquired rifampin 600 mg twice day by day for 4 weeks, and 32 obtained placebo. Patients (n = 106) received fluconazole 200 mg day by day, and 103 obtained placebo for 6 weeks. Healing was complete in 79% of the fluconazole group and 34% of the placebo group at 3 months, followup. Comparison of oral itraconazole and intramuscular meglumine antimoniate in the treatment of cutaneous leishmaniasis Saleem K, Rahman A. Itraconazole (100 mg twice daily for 6�8 weeks) was superior to meglumine antimoniate in achieving complete scientific and parasitologic treatment (75% in contrast with 65%), with fewer side effects. Patients (n = 120) had been handled with cryotherapy as soon as weekly over one to seven sessions; 84% of lesions have been cured after one to four sessions. A single localized therapy with thermotherapy was more effective than 5 days of intralesional glucantime. Also, thermotherapy was value efficient, with fewer unwanted aspect effects, and better patient compliance than intralesional glucantime. In an open-label trial, one group obtained oral miltefosine 50 mg every day for 28 days, and the other group obtained thermotherapy of 50�C on the lesion and perilesional space. This was a randomized, double-blind, controlled examine of 10% and 15% hypertonic saline injections compared with that of sodium stibogluconate. Ninety patients have been enrolled; 60 obtained miltefosine orally and 30 received pentavalent antimony. Apoptosis-like death of Leishmania donovani could also be a potential explanation of the mode of action of miltefosine. Role of imiquimod and parenteral meglumine antimoniate in the initial remedy of cutaneous leishmaniasis Arevalo I, Tulliano G, Quispe A, Spaeth G, Matlashewski G, LlanosCuentas A, et al. Imiquimod kills the intracellular Leishmania amastigotes in vitro by activating macrophages to launch nitric oxide. Topical paromomycin with or with out gentamicin for cutaneous leishmaniasis Ben Salah A, Ben Messaoud N, Guedri E, Zaatour A, Ben Alaya N, Bettaieb J, et al. Treatment continued for 20 days; treatment charges have been 81%, 82%, and 58% for the paromomycin�gentamicin, paromomycin, and management groups, respectively. Comparison between the efficacy of photodynamic therapy and topical paromomycin in the therapy of Old World cutaneous leishmaniasis: a placebo-controlled, randomized scientific trial Asilian A, Davami M. The parasiticidal effect of electrical energy on Leishmania main, both in vitro and in vivo Hejazi H, Eslami G, Dalimi A. Three weeks of electrotherapy at 3 V for 10 minutes twice weekly appeared to treatment all of the lesions in mice. Thirty-five sufferers acquired meglumine antimoniate, and 31 obtained intralesional zinc sulfate. One group acquired intralesional antimony along with pentoxifylline, and the other received antimony with placebo. Cure rate was higher in the pentoxifylline group, but not statistically important. Liposomal amphotericin B therapy of cutaneous leishmaniasis due to Leishmania tropica Solomon M, Pavlotsky F, Leshem E, Ephros M, Trau H, Schwartz E. Thirteen sufferers acquired liposomal amphotericin B (5 consecutive days of three mg/kg, adopted by a sixth dose on day 10); 85% had facial lesions. The widespread atypical melanocytes often originate on the top or neck and spread slowly. The differential prognosis includes solar lentigo, macular seborrheic keratosis, pigmented actinic keratosis, pigmented squamous cell carcinoma in situ, and pigmented superficial basal cell carcinoma. Excisional biopsy of the complete lesion is right in order to ascertain its most depth. However, the lesion tends to be large (>1 cm) because of its propensity for in depth radial development before vertical progress into the dermis. Treatment is primarily surgical, though eradication by other methods may be thought-about. Biopsy of sufficient depth is important for prognosis and management of pigmented lesions. Evaluation ought to embrace a private and family history, full skin examination, and palpation of regional lymph nodes.
Premarin 0.625 mg quality
An uncommon giant scalp seborrheic keratosis was successfully handled with topical fluorouracil women's health clinic saskatoon order premarin 0.625 mg line. A topical 50% urea-containing product utilized under occlusion was combined with superficial scraping to remove hyperkeratotic seborrheic keratoses on the trunk and extremities menstruation and anxiety premarin 0.625 mg generic. It can affect both humans and animals and is prevalent worldwide, however is extra frequent in the tropics. Infection is usually sporadic, however outbreaks could happen because of contaminated soil and wooden. Infection is subsequently more common in some occupations 2598 such as horticulturists, carpenters, and miners. The preliminary lesion seems at the website of damage as an erythematous, ulcerated, or verrucous nodule. It is also inexpensive and is the first-line remedy for sporotrichosis in most growing nations. It must be initiated at a loading dose of 200 mg thrice daily for 3 days followed by a hundred to four hundred mg every day. Cure rates for cutaneous and lymphocutaneous an infection are high, typically 90% to 100%. Fluconazole (400�800 mg daily) remedy gives response charges of 63% to 71% and therefore is really helpful for second-line therapy only. On the basis of case reviews, parenteral amphotericin B (AmB) is the preferred treatment (AmB deoxycholate 0. After AmB induction remedy, itraconazole (200 mg twice daily) is given as maintenance remedy. Thermotherapy (using infrared and much infrared wavelengths to heat 2599 tissues to 42��43�C) is known to be efficient, although there are few stories of its use. Clinical knowledge demonstrating the potential of cryotherapy as an adjuvant to systemic remedy are restricted. Culture is the most delicate means of diagnosis and is characteristically rapid, with growth often seen inside 1 week in 90% of cases. In the remaining 10% it might take as much as four weeks to achieve a optimistic result on Sabouraud agar tradition. The analysis is confirmed by demonstrating dimorphism, or conversion to the yeast part. Mortality was 30% and significantly higher in those with central nervous system involvement and death. In this group of patients amphotericin B was normally the drug of alternative, and itraconazole was used as maintenance remedy. The patients acquired amphotericin and itraconazole combination remedy for sporotrichosis. They required treatment with several-month programs of systemic corticosteroids along with continued antifungal remedy. The authors famous that illness relapsed when corticosteroids have been discontinued prematurely. This evaluation reviews that saturated solution of potassium iodide is generally used as a first-line treatment selection for uncomplicated cutaneous sporotrichosis in resource-limited nations. Itraconazole has excellent efficacy and is beneficial for the treatment of all forms of sporotrichosis. Amphotericin B is used initially for the therapy of extreme or systemic disease, during being pregnant, and in immunosuppressed sufferers followed by itraconazole prophylaxis if indicated. This article evaluations the pharmacology and opposed results of potassium iodide as a therapeutic agent. It discusses contraindications to its use, which embody a history of thyroid or kidney disease and being pregnant. A male grownup patient developed disseminated infection after therapy with multiple immunosuppressants, including etanercept and infliximab for inflammatory arthritis. Treatment was given till cure, and the median therapy period was 12 weeks (range 2� sixty four weeks). Lymphocutaneous and disseminated forms required approximately 2 weeks longer to obtain treatment than did the fastened form. One patient, regardless of dose escalation of itraconazole to 400 mg/day, failed 2602 and was cured only after switching to potassium hydroxide. This examine demonstrated that a dose of one hundred mg day by day is extremely efficient within the overwhelming majority of sufferers with fixed or lymphocutaneous disease, although it was sometimes related to a better risk of relapse. This is essential because it makes itraconazole a more affordable choice in resource-poor areas. This report has additionally demonstrated that potassium iodide could be more efficacious than itraconazole, though there have been no comparative research. This randomized controlled trial evaluating pulse itraconazole 200 mg twice every day for 1 week every month (n = 25, mean course of treatment 2. Pulse therapy has the advantages of decrease value and fewer adverse results, although this small trial demonstrates larger efficacy with the continuous itraconazole regimen. One hundred and three instances of the lymphocutaneous and stuck cutaneous sorts of sporotrichosis are described during the interval 1990 to 2002. Potassium iodide was used as first-line therapy, and in 93% of sufferers therapeutic of lesions occurred in four to 32 weeks (average eight. This research demonstrates that the efficacy of potassium iodide is corresponding to itraconazole. The authors also level out that one of many advantages of terbinafine is that it has fewer drug�drug interactions than does itraconazole. Itraconazole 100 mg daily and terbinafine 250 mg given to 249 and fifty five patients, respectively, with culture-proven sporotrichosis demonstrated nearly equal treatment rates in each groups of 92% to 93% within an analogous mean period (11. Adverse effects had been equally frequent with both drugs, occurring in approximately 7% of those handled and were generally delicate besides in two patients receiving itraconazole who had to discontinue therapy. This research offers additional evidence for the efficacy of lower doses of itraconazole or terbinafine remedy. This clinical trial concerned 14 sufferers with lymphocutaneous an infection and sixteen with osteoarticular or visceral sporotrichosis. Eleven of the 30 patients had previously been handled with different types of antifungal therapy with out success. Four patients received fluconazole 200 mg/day, and one other four obtained 800 mg/day. Seventy-one percent of patients (10/14) with lymphocutaneous sporotrichosis had been cured. However, solely 31% (5/16) with osteoarticular or visceral sporotrichosis responded to remedy.
Premarin 0.625 mg generic
Preoperative workup consists of historical past of prior remedy women's health center peru il 0.625 mg premarin otc, clinical size of the lesion menstruation for dummies cheap 0.625 mg premarin with amex, and an correct histopathologic analysis. A shave biopsy is mostly sufficient for epidermal and deep dermal inspection, however punch biopsy to subcutaneous fats or an incisional or excisional biopsy can generally provide further information. For causes of prognostication, the pathology report should touch upon depth of tumor invasion, histologic differentiation, and the presence or absence of sclerosis, single cell infiltration, and neurotropism. High-risk tumors are recurrent; have a diameter of more than 2 cm; are current on the ear, temple, lip, or anogenital area; or have poor histologic differentiation or other histologic features famous earlier. In this method marginal, normal-appearing pores and skin is eliminated as a thin tangential layer round and beneath the clinically obvious tumor, exactly oriented, horizontally sectioned, and instantly processed as a frozen section for histologic analysis. Surgical margins of four to 6 mm are often sufficient to achieve a 95% likelihood of a cure. A margin of 3 to 4 mm across the tumor should be included in the remedy area to ensure full removing of the tumor. Treated lesions typically require a number of weeks to 2610 heal and may go away a white atrophic or hypertrophic scar that can be cosmetically unappealing. Cosmetically sensitive areas, concave surfaces, and skin prone to keloid formation or poor wound therapeutic must be prevented. Cryosurgery destroys a tumor if it is frozen to -60�C, achievable with timed phases or using thermocouples. It leaves a wound that may blister and drain however otherwise heals without complication to a porcelain white atrophic scar. It has the advantage of being fast, simple, and inexpensive, however the success of the process is very much operator dependent. Complications embrace hypopigmentation, telangiectasia, lack of adnexae, radiation dermatitis, and the looks of a new primary tumor 10 to 20 years later. Brachytherapy has just lately been extensively used because of the ability to deliver vitality at a highdose price, resulting in fewer affected person visits. Patients with immunosuppression can have a higher recurrence fee and require close surveillance. Margins of no less than 6 mm have been proposed for tumors 2 cm, histologic grade 2, with invasion of subcutaneous tissue, and/or location in high-risk areas. The first examine discovered no important distinction in treatment rates between curettage and electrodesiccation (14 of 14 cases successfully treated) and excision (15 of sixteen successfully handled and 1 recurrence). The second examine discovered the curettage and electrodesiccation cure price (106 of 106 successfully treated) to be considerably larger than an arbitrary treatment rate of 95%. No tumor recurred after 1 yr of follow-up, and one recurrence occurred within the 5-year interval, for a 99% recurrence-free finish point. Radiation therapy is generally reserved for patients over 50 years of age because of the potential long-term sequelae. Consecutive samples have been taken from all 495 patients with 616 main nonmelanoma pores and skin cancers recognized in 1999 and 2000. Recurrent tumors were detected earliest after curettage and electrodesiccation (1. High-risk cutaneous squamous cell carcinoma with out palpable lymphadenopathy: is there a therapeutic role for elective neck dissection Clearance charges various by drug routine, and a lot of the studies lacked long-term follow-up. Adverse occasions have been uncommon, with two stories of pancytopenia in patients with chronic renal failure. A complete evaluate on intralesional brokers and their function in cutaneous neoplasms. Third-Line Therapies 2620 Acitretin suppression of squamous cell carcinoma: case report and literature evaluation Lebwohl M, Tannis C, Carrasco D. A evaluate of the literature on vulnerable individuals, such as organ transplant recipients and people with xeroderma pigmentosum. In healthy infants mortality is rare, with reported charges up to 3%, contrasting with up to 50% to 60% in adults with comorbidity. Death happens because of complications such as pneumonia, hypovolemia, electrolyte imbalance, and sepsis. Tender erythema is adopted by superficial, flaccid blistering, most pronounced in flexural and periorificial areas, sparing mucosal surfaces, and starting from localized blisters to widespread exfoliation. This leads to impaired thermoregulation and fluid stability and susceptibility to sepsis and secondary infection. Bullae rupture to depart denuded pores and skin, followed by reepithelialization with out scarring. Histology of 2624 affected pores and skin usually reveals a superficial subcorneal blister; absence of epidermal necrosis and minimal inflammation. A frozen section of blister roof can affirm the superficial stage of cleavage, facilitating a more rapid prognosis. The main differential analysis is the Stevens�Johnson syndrome� toxic epidermal necrolysis spectrum, by which distinguishing options embrace targetoid pores and skin lesions, mucosal involvement, and subepidermal stage of blistering with full-thickness epidermal necrosis. Additional differential diagnoses in infants include hereditary circumstances similar to epidermolysis bullosa, epidermolytic ichthyosis, and bullous mastocytosis. Management Strategy Treatment includes antibiotic remedy in combination with supportive measures addressing electrolyte and fluid balance, temperature regulation, nutrition, analgesia, and skin care. Bland emollients similar to 50:50 white gentle paraffin/liquid paraffin should be utilized often to scale back friction and insensible fluid losses. Nonadherent dressings are used to cover denuded areas, with avoidance of adhesive tapes directly on pores and skin. Systemic -lactamase�resistant antibiotics are essential to eradicate the causative S. Strict infection control measures are advisable, together with patient isolation, barrier nursing, and scrupulous handwashing. Nosocomial staphylococcal scalded skin syndrome brought on by intraarticular injection Emberger M, Koller J, Laimer M, Hell M, Oender K, Trost A, et al. Infection control measures (patient isolation, barrier-nursing, chlorhexidine handwashing, remedy of carriers with nasal mupirocin, and chlorhexidine showers) controlled the outbreak. Adult case of staphylococcal scalded skin syndrome differentiated from poisonous epidermal necrolysis with assistance from dermoscopy Miyashita K, Ogawa K, Iioka H, Miyagawa F, Okazaki A, Kobayashi N, et al. Dermoscopy as a diagnostic software was utilized to show superficial degree of cleavage at a contemporary exfoliation site; subcorneal detachment was subsequently confirmed histologically. A health care employee with continual hand dermatitis was recognized because the source of the outbreak after mass screening involving multisite swabbing and pooled, enrichment culture. Mild staphylococcal scalded skin syndrome: an underdiagnosed scientific dysfunction Hubiche T, Bes M, Roudiere L, Langlaude F, Etienne J, Del Giudice P.
Real Experiences: Customer Reviews on Premarin
Ugrasal, 64 years: Two sufferers given oral pyridoxine dosages various from one hundred mg to 1 g/day reported increased sunlight tolerance. Gonococcal ophthalmia is strongly suggested when typical gram-negative diplococci are recognized in conjunctival exudate, justifying presumptive treatment after applicable cultures have been obtained. Pyogenic granuloma that responded to native injection of steroid Niiyama S, Amoh Y, Katsuoka K. Side results were restricted to erythema and edema around treated lesions, necrosis of handled lesions for 2�3 weeks, and sore muscles at time of pulse supply.
Marlo, 43 years: Excellent evaluate of different and concomitant psychotropic medicines, together with clomipramine, venlafaxine, buspirone, and pimozide. Although the decision of mastocytomas could occur with or with out therapy, the time to decision is faster with treatment using topical 1653 glucocorticoids, which are effective and secure contemplating the very lengthy time for resolution. Eight patients were given colchicine, 5 of whom showed complete remission within four to 6 weeks. The retention mucocele is more apt to happen on the buccal cheek or soft palate of an older affected person.
Ines, 24 years: Acitretin doses of 30 mg day by day have been used, resulting in mucocutaneous unwanted effects (dryness of the mouth, lips, nostril, and pores and skin and hair loss) and hyperlipidemia. A bacteriology swab from lesional pores and skin is suggested to decide tradition and sensitivity as bacterial resistance is common. Glossodynia from Candida-associated lesions, burning mouth syndrome, or mixed causes Terai H, Shimahara M. A 64-year-old man with both psoriasis and bullous pemphigoid failed mycophenolate mofetil therapy and was started on prednisone 60 mg/day.
Tamkosch, 63 years: Pruritus decreased after 2 weeks, and skin lesions resolved within 2 months, leaving solely hyperpigmentation. Lasting remissions were seen in 70% of these utilizing the tape versus 25% of these utilizing topical corticosteroids with out occlusion. Naltrexone at a dose of fifty mg every day managed the condition in two patients with aquagenic pruritus to whom it was given. Arg94Gly) of keratin 17 in a Chinese household with steatocystoma multiplex Zang D, Zhou C, He M, Ma X, Zhang J.
Kapotth, 48 years: Rituximab for the treatment of lupus erythematosus panniculitis Moreno-Suarez F, Pulpillo-Ruiz A. Of the 12 patients with one of the best response, 6 had a recurrence after a dosage reduction or discontinuation. All sufferers responded with a imply reduction in wound measurement of 79% after eighty four to 126 days without any opposed effects. Among patients with recurrent an infection, some knowledge suggest that decolonization can reduce the speed of future recurrences.
Nerusul, 33 years: Pyogenic granuloma that responded to native injection of steroid Niiyama S, Amoh Y, Katsuoka K. In 389 sufferers, topical 40% silver nitrate paste was utilized after 2% lidocaine gel; 70% cleared after one software, 97. Because methotrexate and ciclosporin are immunosuppressive, they should be used cautiously with biologics and for as brief a period of combination as possible. Photothermolysis utilizing light with selected wavelengths may cut back persistent hypertrichosis.
Einar, 50 years: It has shorter irradiation times, no need for protecting glasses after therapy, and lowered threat of photocarcinogenesis. Intralesional corticosteroids, aluminum hydroxide dietary supplements, bisphosphonates, diltiazem, colchicine, and probenecid have shown success, largely in calcinosis associated with dermatomyositis. In addition, elevated antibody titers persist for a number of years after preliminary an infection. This Cochrane evaluation summarizes the obtainable evidence with regard to 5 randomized-controlled medical trials (representing 23 publications) involving agalsidase- and agalsidase-.
10 of 10 - Review by B. Gorn
Votes: 295 votes
Total customer reviews: 295